Key Takeaways
• Restoring energy balance reverses Alzheimer's symptoms ||| • Mouse models show improved brain function with intervention ||| • Energy metabolism crucial for Alzheimer's progression ||| • Targeting brain metabolism offers broad therapeutic benefits
Researchers have recently demonstrated that restoring energy balance to mouse brain models can effectively combat neurological and behavioral symptoms associated with Alzheimer’s disease. Their studies demonstrate the feasibility of taking an integrative metabolic approach — one focused on how cells process energy — as a potential route towards therapeutic development for Alzheimer’s.
Why Energy Balance Is Key for Alzheimer’s
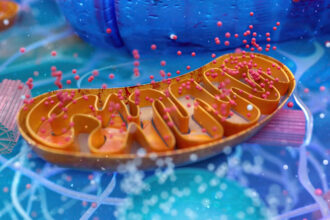
Healthy brain cells rely on consistent energy supplies in order to function normally; with Alzheimer’s disease, this supply becomes compromised; neurons find it increasingly challenging to generate and use energy efficiently, contributing to cognitive decline and disease progression. Instead of simply looking at classic hallmarks like amyloid plaques or tau tangles as indicators, this research seeks to understand how Alzheimer’s affects cellular energy systems and alters them accordingly.
Researchers Who Explore the Mouse Model
Scientists employed mouse models genetically predisposed to Alzheimer’s-like pathology and cognitive impairment in order to simulate Alzheimer’s-like symptoms in humans, such as memory problems and metabolic disruption in their brains. These animals provided invaluable insight into human disease conditions such as Alzheimer’s and related dementias.
Researchers attempted a novel approach in their quest for biochemical imbalance: they restored metabolic function. By altering how neurons processed energy — specifically by improving efficiency of cell machinery responsible for creating it — researchers witnessed both biological and behavioral improvement among mice.
Striking Improvements in Brain Function
After restoring energy balance in Alzheimer’s model mice, key cognitive behaviors improved significantly – suggesting memory and learning deficits had not only been delayed but actually mitigated as a result of metabolic intervention.
At a cellular level, neurons appeared healthier, with energy production pathways working more normally – suggesting that proper energy metabolism is not just an unwitting participant in Alzheimer’s development but can actually accelerate it and worsen symptoms of Alzheimer’s.
Why This Research Is Engaging
This work shifts attention from protein aggregates alone, towards exploring how cellular energy dysfunction contributes to Alzheimer’s disease. If energy imbalance is indeed the key factor leading to neuron degeneration, therapies which support brain metabolism could have significant long-term benefits by stopping or even reversing disease processes more broadly.
Targeting metabolism also allows other approaches, including lifestyle interventions (diet and exercise) known to influence brain energy management, to combine.
What this Means for Humans
While results in mice are promising, translating them to humans will require time and investigation. Mouse models provide invaluable insights into mechanisms and potential treatments pathways; however, human biology is far more intricate. Researchers must investigate whether similar metabolic restoration can be achieved safely and effectively among people.
Still, this concept – that improving brain energy balance could reverse cognitive decline — marks an important advance in Alzheimer’s research and points toward potential drug targets for future drug development efforts.